Contact us today
Women and Secondary Conditions: What SCI Awareness Month Doesn’t Always Talk About
Every September, during SCI Awareness Month, social media is filled with familiar stories: the moment everything changed, the first time using a wheelchair, learning to navigate a world that wasn’t built for you. These stories matter deeply, but they’re not the whole journey.
What often gets left out are the everyday struggles: the UTI that cancels your weekend plans. The way your period decides to completely rewrite the rules. The bladder control issues that make you second-guess every outing. These secondary conditions don’t just disrupt your plans; they shape how you live, connect, and show up in the world.
At HerSpine Solutions, we believe in telling the complete story, including the unglamorous parts. Because these challenges are not side notes; they’re daily realities that deserve real attention, honest conversations, and practical solutions.

Urinary Tract Infections (UTIs)
For many women with SCI, UTIs aren’t just an occasional nuisance; they can become a recurring, exhausting part of life. And unlike non-disabled women, symptoms don’t always show up in the “classic” way. Instead of burning or odour, you might notice cloudy urine, increased spasticity, chills, or even just feeling unusually tired. That’s why it’s important to really know your body and recognise your personal early warning signs.
The truth is, these infections aren’t about being “dirty” or “careless.” They often happen because nerve damage affects bladder emptying, leaving behind urine that gives bacteria a chance to thrive. Catheter use, reduced mobility, or hormonal changes (like around your period) can also increase the risk.
While you may not be able to stop UTIs altogether, you can take steps to reduce how often they happen and lessen their impact on your life.
Practical Tips:
a). Empty your bladder fully and regularly, using techniques or catheters that work best for you. Incomplete emptying is one of the biggest culprits.
b). Hydrate smartly; water helps flush bacteria, but balance it with your bladder management routine so you’re not overfilling your system.
c). Notice your warning signs; whether that’s fatigue, spasms, or urine changes. Catching an infection early makes a big difference.
d). Rethink hygiene gently; daily washing with mild soap and water is enough. Skip harsh feminine washes, wipes, or scented products that can upset your balance.
e). Work with your doctor; some women benefit from low-dose preventative antibiotics, bladder irrigation, or supplements like cranberry/D-mannose, but these should always be personalised.
Pelvic Floor Dysfunction
Think of your pelvic floor as the hammock of muscles that supports your bladder, bowel, and reproductive organs. After a spinal cord injury, the communication between your brain and this support system is disrupted. The result can be unpredictable: bladder or bowel control issues, constipation, recurring pelvic pain, or changes in sexual function that can affect how you feel about intimacy and your own body.
For many women, this is one of the hardest adjustments. It can feel frustrating when your body doesn’t respond the way it once did, but remember, you are not broken. Your body is adapting, and with the right strategies, you can regain confidence and control.
Management Tips:
a). Specialised pelvic physiotherapy: Not all women with SCI can do traditional Kegels. A physiotherapist experienced in neuro-rehabilitation can guide you in exercises or electrical stimulation that fits your level of injury.
b). Pain management: Don’t suffer in silence. Talk to your healthcare provider about options, from analgesics and antispasmodics to nerve pain medications, that can ease discomfort.
c). Diet and digestion: Fibre-rich foods, consistent hydration, and a regular bowel routine can help reduce constipation and the pressure it puts on your pelvic floor.
d). Intimacy and sexuality: Changes in sensation, lubrication, or orgasm don’t mean the end of pleasure. Explore what feels good, use lubricants, and have open conversations with your partner or a sexual health specialist.
e). Whole-body approach: Sometimes strengthening your core, improving posture, or managing spasticity can indirectly support pelvic floor health.
Your pelvic floor may be working differently now, but with patience, tailored care, and support, it’s possible to find new ways of living and thriving with your body.
Pressure Sores
Pressure sores can be sneaky. One moment you’re living your life and the next, a red mark appears suddenly. Of course it’s a cause for concern, and here’s the thing: pressure sores happen when your skin has been under pressure for too long.
When you spend too much time in a wheelchair or bed, certain parts of your body carry more weight and blood flow to that area gets cut off. Next thing, your skin starts protesting, and a wound forms. The most frustrating thing about pressure sores is that you can’t feel them developing, so what starts as a small red mark can turn into something that derails your plans and affects your independence. But pressure sores are largely preventable, and you can have more control over them.
Prevention Tips:
a). Practice moving your body after sitting for 15-30 minutes. Even 30 seconds of shifting can make a world of difference.
b). Check your skin daily for redness, swelling or any wound that hasn’t healed yet. Skin checks aren’t vanity, they are a necessity.
c). Invest in good seat cushions, foams and bed paddings that offer great support and protect your body.
d). If you spend a lot of time in bed, create a regular turning schedule.

Menstrual & Sexual Health Changes
Let’s talk about periods and sex for a minute, because dealing with your monthly visitor when you’re managing SCI can be complicated. Maybe your periods are now irregular, your cramps have intensified, or your flow has changed entirely. Add in the challenges of managing hygiene when bending and reaching aren’t easy anymore, and it’s enough to make anyone feel overwhelmed.
What about the changes in your sexual health? Decreased libido, vaginal dryness, different physical sensations, all shifts that can affect your relationships, your confidence, and how you see yourself as a woman. First, remember that your feelings are completely valid and taking time to figure out your new normal is about being smart.
Management Tips:
a). Use tools that make life easier, like reachable supplies, long handles, and sexual equipment.
b). Work with healthcare providers who understand both SCI and women’s health, not someone who treats you like a medical puzzle.
c). Consider support from physiotherapists and counsellors who can help you understand your body’s changes and explore solutions.
d). Communicate with your partner, family members, and healthcare providers about what you need.
💡 If you need more guidance, read our blog post on how to manage your periods after SCI.
Osteoporosis
Osteoporosis is associated with older people, but bone loss after SCI can happen anytime. When your muscles aren’t being used as much and nerve function changes, your bones can start getting weak especially in your legs, hips, and lower spine. These weakened bones can affect your balance, increase your risk of falls or fractures, and also impact your overall sense of independence. Osteoporosis in SCI can be frustrating because you might not know until a “small” fall causes large effects. That’s why it’s important to take back control of your bone health.
Management Tips:
a). Know your risk factors and go for regular bone density tests which can help you catch problems early.
b). Go for foods rich in calcium, magnesium and Vitamin D, which can help to build the bones.
c). Engage in safe weight-bearing and stability exercises to strengthen your bones.
d). If you need more support, talk to your healthcare professional about medications that support bone health.

Cardiovascular Issues
Think of your autonomic nervous system as the quiet manager that keeps your heart rate and blood pressure steady without you even noticing. After a spinal cord injury, that system may not function the same way. This can lead to unpredictable changes, like sudden drops in blood pressure when sitting up (orthostatic hypotension), dangerous spikes triggered by pain or bladder issues (autonomic dysreflexia), or irregular heart rhythms.
But that’s not the whole picture. The lifestyle changes that often come with SCI, long hours of sitting, reduced physical activity, changes in muscle mass, stress, or limited access to exercise spaces, can also increase the risk of obesity, diabetes, and heart disease over time.
Heart health after SCI requires more intentional care than before. It’s not about “fixing” your body, but about working with it, knowing your risks, listening to your signals, and making choices that keep your heart strong.
Prevention Tips:
a). Stay active in adapted ways: Even small, regular movements matter. Wheelchair aerobics, resistance bands, and arm cycling can boost circulation and heart strength.
b). Watch your blood pressure: Keep track of sudden highs or lows. If you experience symptoms like pounding headaches, dizziness, or flushing, seek medical help; it could be autonomic dysreflexia.
c). Mind your diet: A balanced diet low in processed fats and high in fruits, vegetables, and whole grains helps reduce cardiovascular strain.
d). Manage stress: Breathing exercises, meditation, and peer support can calm your system and protect your heart.
e). Partner with your healthcare team: Routine check-ups, heart monitoring, and tailored exercise programmes can catch issues early.
Supporting your cardiovascular system is about honoring the body that’s carrying you through this journey.
General Management Strategies in SCI
Managing the secondary conditions that come with SCI isn’t about adding more stress to your life, but about creating systems that work for you. Think of it as building your personal support team, with habits, tools, and strategies that consistently have your back.
Maintain Regular Exercise
Exercise doesn’t have to be tough; it just has to keep you active. Start with 15-30 minutes of wheelchair friendly workouts, and have a steady routine that helps with your waist, back, and legs. Talk to a physiotherapist who understands SCI and works on personalized routines. Your body has specific needs, and your workouts should reflect that.
💡If you’re unsure about which to start, read our newsletter on safe and effective workouts for women living with SCI.

Focus on a Healthy Diet
Use your diet to give your body the strength it needs to stay active. Go for anti-inflammatory foods that support healing, incorporate fiber-rich foods for bowel management, add calcium and Vitamin D for bone health, and always stay hydrated even when bladder management feels tricky.
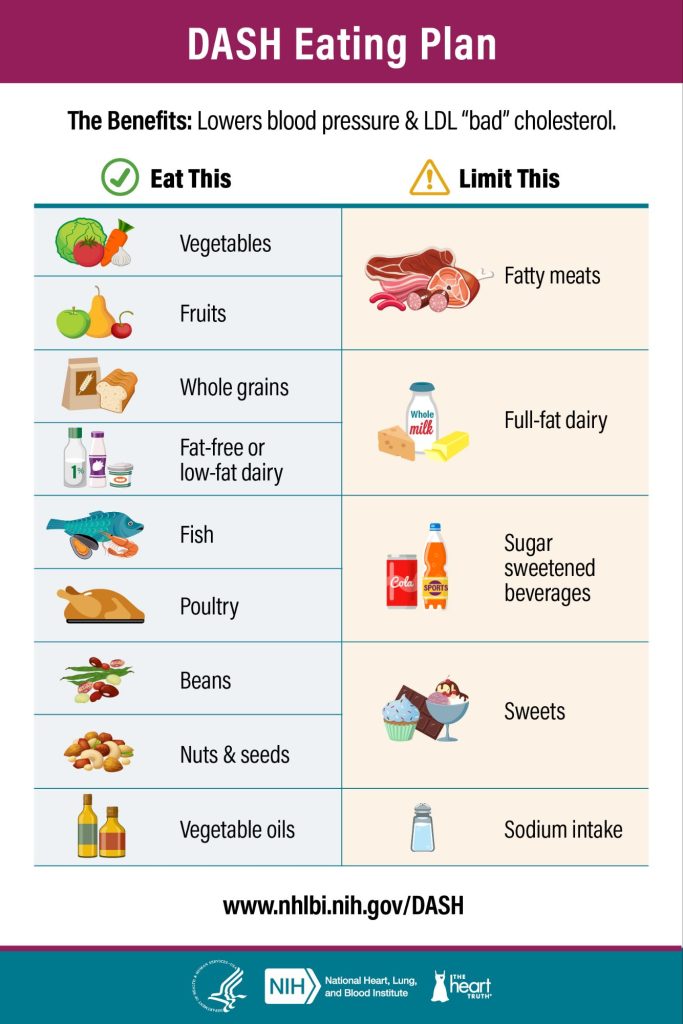
💡If you’re confused on where to start, explore the DASH diet plan with a nutritionist who can modify it for your SCI needs.
Take Your Prescribed Medications
Pill organizers and medication schedules can feel overwhelming, but here’s what you should remember: those medications are working behind the scenes to manage symptoms and prevent complications so you can focus on living. To make it easier:
a). Set reminders to help with medication schedules
b). Keep a record of how medicines affect you
c). Discuss any concerns with your health providers
d). Do your own research, but don’t self-medicate.
Connect with Others
Living with SCI doesn’t mean living in isolation, especially when you’re managing conditions that can make you feel alone. Connecting with women who understand your daily realities and can share new knowledge can be transformative to your mental health.
That’s why the HerSpine Virtual Ladies Lounge exists. An online space with women who understand why managing secondary conditions can feel harder than the initial injury. Every two weeks, we share experiences, celebrate small wins, and support each other through the unique challenges of living with SCI.
Join our next meeting here and discover what it feels like to talk about secondary conditions and actually be heard. Because some conversations are easier when you’re surrounded by women who get it.
Conclusion
This September and every month after, we’re rewriting the narrative. Because living with SCI isn’t just about the initial injury story or the recovery time; it’s about navigating the secondary conditions with knowledge, support, and the confidence that you’re not alone.
You’re not being dramatic when a UTI spoils your week, and you’re not alone when menstrual changes add another layer of stress to your life. These challenges are real, and they deserve to be discussed openly. You deserve healthcare providers who take your concerns seriously, communities that understand them, and resources that help you manage them effectively.
Remember: You’re not just managing conditions, you’re redefining what it means to live fully after SCI.
💡Join the conversation by subscribing to our LinkedIn newsletter for weekly insights, real stories, and practical advice for women living with SCI.
FAQs
1. What should I do if I have signs of UTI?
Classic UTI signs include painful urination, dark or cloudy urine with a strong odour, fever, and lower back pain. But if something feels off, don’t wait for a sign. Speak to your healthcare provider and get a urine test done. UTIs can escalate quickly in people with SCI, so early intervention is your best strategy.
2. How can I monitor my heart health?
Make regular checkups a part of your routine. Go for blood pressure measurements, blood sugar tests, pulse checks, and electrocardiograms. Keep a simple log of your readings and don’t ignore symptoms like chest pain, fatigue, dizziness, or swelling. If these happen, see a healthcare professional immediately.
3. What is the DXA bone test?
The DXA bone density test is like an X-ray that checks your risk of osteoporosis by measuring the level of calcium and other minerals in your bones. For women with SCI, this painless test is helpful since it can detect weak bones and reduce the risk of fractures.
💡Do you need more information? The Spinal Injuries Association provides comprehensive fact sheets, tips, and practical guidance on how to live with spinal cord injury.
